
To access the carrier product and rate information provided by PRISM, check the box below indicating you have read and agree to the license agreement. A button will then appear to access PRISM.
This site uses cookies to track your agreement option. If the terms of the license agreement change or if you clear the cookies from your browser, this page will appear once again during the PRISM login process.
Starting July 1, Covered California for Small Business (CCSB) is offering new Blue Shield plans, providing more options for enrollees. These plans include the Access+ HMO Network with Platinum, Gold, and Silver metal tier options, as well as the Bronze Trio HMO 7000/70. The two most popular Blue Shield High Deductible Health Plans (HDHP), Silver Full PPO Savings 2300/25% and Bronze Full PPO Savings 7000 plans, are also now available.
All of these plans offer benefits such as Wellvolution, Teladoc Mental Health, Nurse Help 24/7, LifeReferrals 24/7, and the Blue Card program for when members are outside of California.
For assistance, please contact our Quotes team at quotes@claremontcompanies.com or 800.696.4543.
Login To PrismAverage premiums for employer-sponsored health insurance jumped 7% for both individual and family plans this year — a significant increase after last year’s negligible growth. As disclosed in the 2023 Kaiser Family Foundation (KFF) survey, rising employer healthcare premiums have resumed, a reminder that while there has been great progress expanding coverage, people continue to struggle with medical bills.
The 25th annual KFF 2023 Employer Health Benefits Survey, conducted between January and July 2023, of 2,133 randomly selected private and non-federal public firms of three or more workers, provides a detailed look at trends in employer-sponsored health coverage, including premiums, employee contributions, cost-sharing provisions, offer rates, wellness programs, and employer practices. This year’s report also looks at abortion coverage, mental health and substance use services, and wellness programs.
Check out the KFF 2023 Employer Health Benefits Survey to stay updated on the latest employer-sponsored coverage trends and help employers recruit and retain workers with quality plans that employees value. Contact us today to develop tailored benefits solutions that address your clients’ needs.
KFF 2023 Employer Health Benefits Survey
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
According to the recently released Ease 2023 SMB Benefits and Employee Insights Report, that focuses on the evolving benefits landscape for businesses with 1-250 employees, the smallest businesses are seeing the biggest medical premium increases. The report also offers insights into the benefits pressures employers and employees face and shares data to help you and your clients make informed decisions for the coming year.
With anonymized data collected from more than 2,300 health insurance agencies, 85,000 businesses, and 3.4 million+ employees nationwide that use Ease, the Report found medical premiums continue to climb, employees today expect their organizations to recognize their lives inside and outside of work, and employers and employees are asking more and more of each other.
A cooling job market, hints of a coming recession, unclear return-to-office plans, supply chain disruptions, and inflation, will continue to be challenging for small-to-medium businesses (SMBs).
Brokers who succeed will be the ones who stay out in front and offer benefits that matter to their clients – all while keeping an eye on the bottom line. To do this, they must rely on data-driven insights to learn from what’s come before and what could come next.
You’ll Find Features Insights and Trends On:
Medical premiums are experiencing cost increases much like everything else. Since 2018, individual premiums saw a 21% increase, while family premiums have a slightly lower increase at 17.87% over the same time period. That’s a $104 per month increase for individuals and a $231 per month increase for families — or $1,248 and $2,772 per year — significant for any household.
While the jump in average premiums from 2021 to 2022 fell under the 6.5% rate of inflation, the smallest employer groups were dealt the hardest blow. Employers with only 1-10 employees saw an increase of 12.07%. That’s nearly double the rate of inflation and the largest increase this segment has experienced in the past four years.
Continuing the trend seen since 2018, the smaller the company the more their employees paid toward benefits. Employees working for companies with 101-250 employees paid 37% less than those working for companies with 1-10 employees this past year.
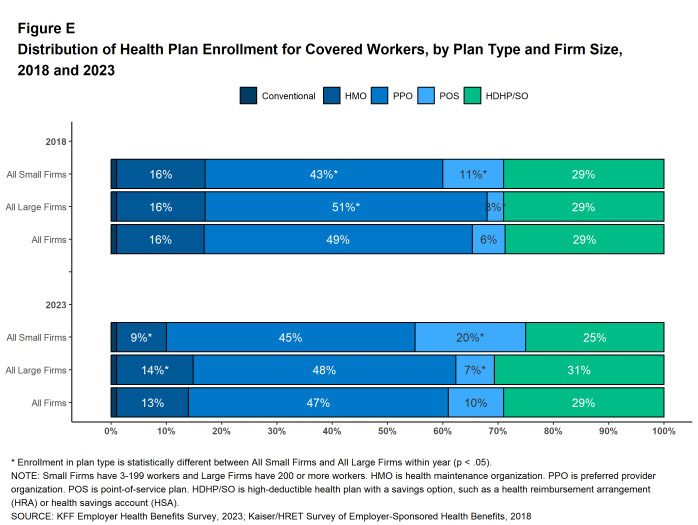
When it comes to plan-type adoption, HMOs and PPOs remain the most popular choice for employees, more than 50% of SMB employees opted to waive coverage entirely, up 13% from 2020.
Though the uptake of consumer-driven health plans remains a small slice of the pie, participation in High Deductible Health Plans (HDHPs) has increased 68% year-over-year. Panning out, HDHPs typically combine with a Health Savings Account (HSA). Given the current state of the economy, households may be opting to use higher deductible plans to save money on their monthly premiums in spite of the higher financial risk if a major medical event occurs. More money in their pockets each month seems like a safer bet.
On average, businesses with more employees offered more medical plans than those with fewer employees in 2022.
Non-medical voluntary benefits offer SMBs a unique way to meet the needs of their employees without destroying their budgets. Must-haves like dental, vision, and life top the list for SMB employees, but lifestyle benefits like financial wellness, legal services, and pet insurance continue to gain steam.
Vision coverage continues to see a decrease year-over-year in premium cost. Short-term disability saw the biggest jump from 2020 to 2022 at almost 12% ($2.75 per month, or $33 more annually).
Similar to the trend seen with medical plans, the larger the company, the more voluntary benefits plans offered per employee in 2022.
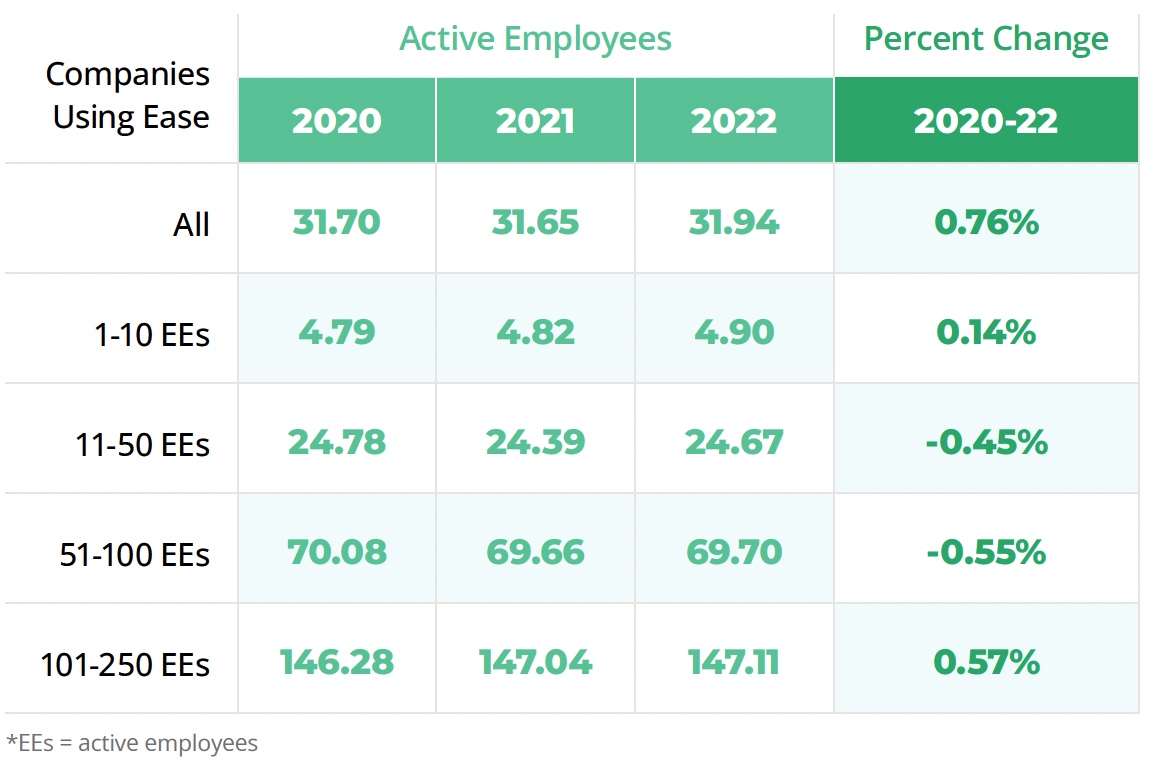
Groups in Ease experienced a nominal increase in the average number of employees. While all segments have seen a small uptick in employees from 2021 to 2022, all fluctuations are within one point when looking at a three-year trend line. Outside of Ease, SMBs experienced a net job loss of 3 million,* or a shrinking of 5% of the total workforce.
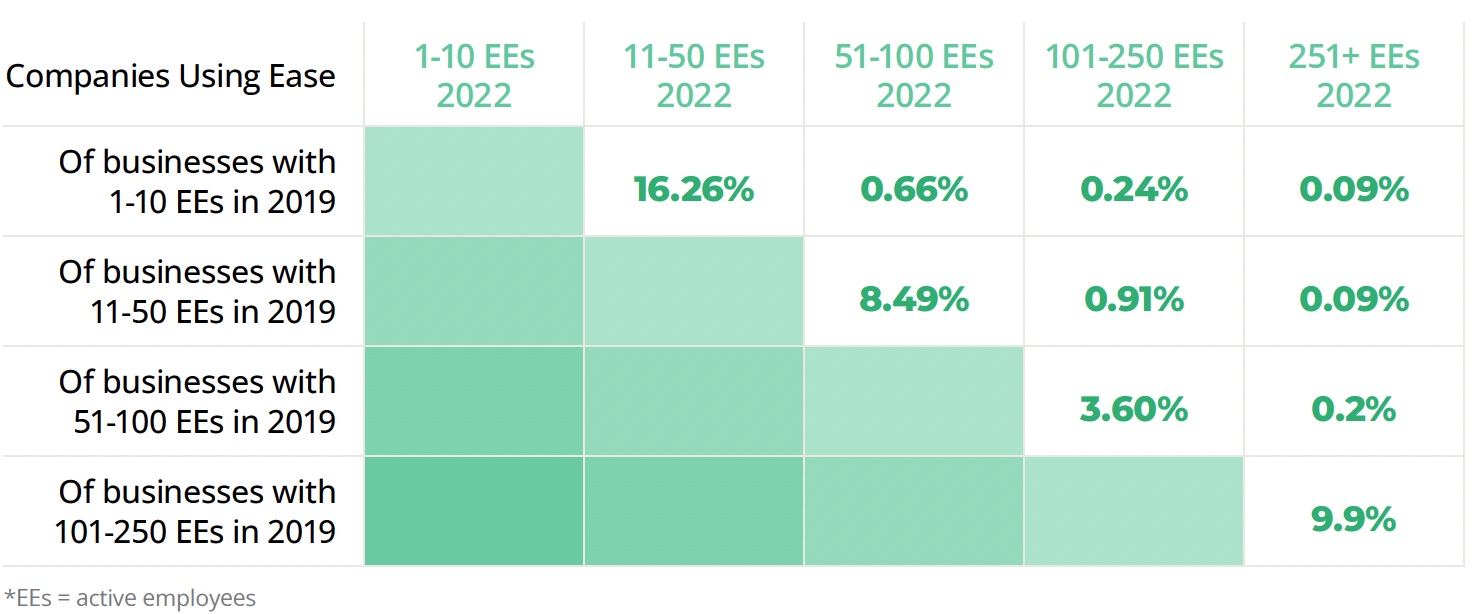
Ease looked at companies using their system since 2019. Overall, 13.29% of companies using Ease grew, while 7.68% shrank over the same period.
By using the data from Ease’s survey of 1,000 U.S.-based employers and employees, you’ll be able provide options and ongoing management support year-round to recession-proof your business.
Employers (ERs) and Employees (EEs) top benefits priorities in 2023:
Employer expectations for year-round support continue to increase. In fact, only 6% of employers surveyed think their broker is needed only during open enrollment. That means 94% expect consultation, innovation, and ongoing management support year-round.
37.52% of agencies offered more support to clients this year than last year by helping them onboard new hires online, conducting benefits elections remotely, and providing compliance support.
78% of agencies anticipate their groups wanting more insurance options this upcoming enrollment season:
73.77% of employers believe benefits administration technology is a higher or equal priority going into this year’s open enrollment.
For a deeper understanding of the latest employee benefits trends and to better advise your clients, download the Ease 2023 SMB Benefits and Employee Insights Report.
Ease is an online benefits enrollment system that makes it simple for insurance brokers and small business employers to set up and manage benefits, onboard new hires, stay compliant, and offer employees one destination for all their human resources information.
The Ease Marketplace is equipped with products, technology solutions, and resources to help you stay ahead of industry trends, defend against new competitors, and build a robust HR offering.
Don’t have an Ease account?
Contact us for free Ease online enrollment for your groups with one line of coverage or more.
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
*U.S. Small Business Administration Office of Advocacy, 2022 Small Business Profile Infographic
Given today’s tight labor market and rising wages, employers are concerned about the cost of health premiums, especially since recent inflation suggests larger increases are imminent. And as disclosed in the Kaiser Family Foundation (KFF) survey, employers continue to be anxious about meeting the mental health needs of their employees and their dependents.
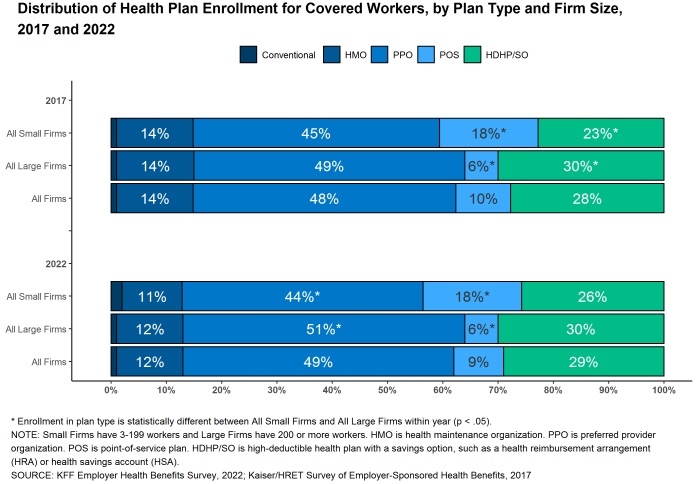
Conducted from February through July 2022, the KFF 2022 Employer Health Benefits Survey, of 2,188 randomly selected private and non-federal public firms of three or more workers, reveals that workers at small firms pay more in premiums and face higher deductibles than workers at large firms.
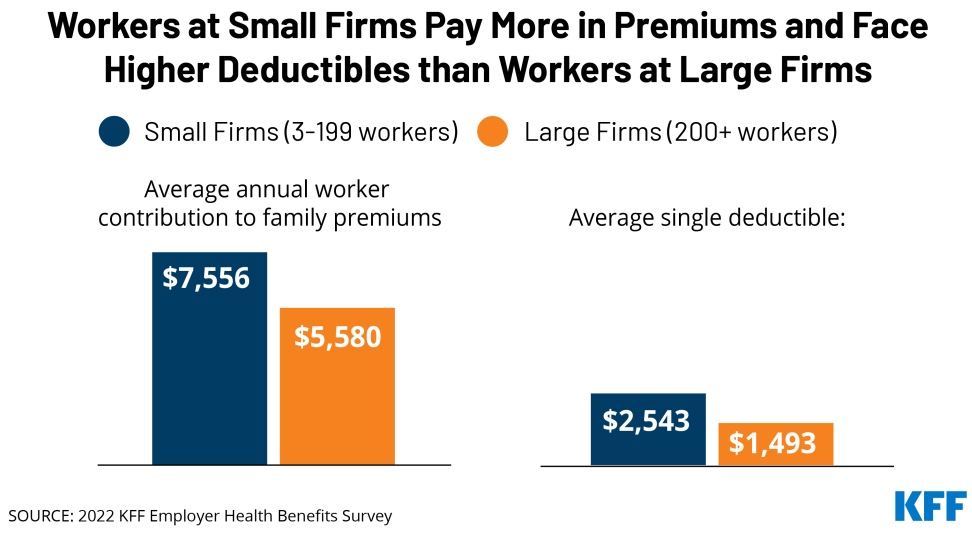
In 2022, the average annual premiums for employer-sponsored health insurance are $7,911 for single coverage and $22,463 for family coverage. In contrast to the lack of premium growth in 2022, workers’ wages increased 6.7% and inflation increased 8%.
Check out the KFF 2022 Employer Health Benefits Survey to ensure that you and your clients are up to date with the latest employer-sponsored coverage data. Contact us today to develop tailored benefits solutions that address your clients’ needs.
KFF 2022 Employer Health Benefits Survey
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
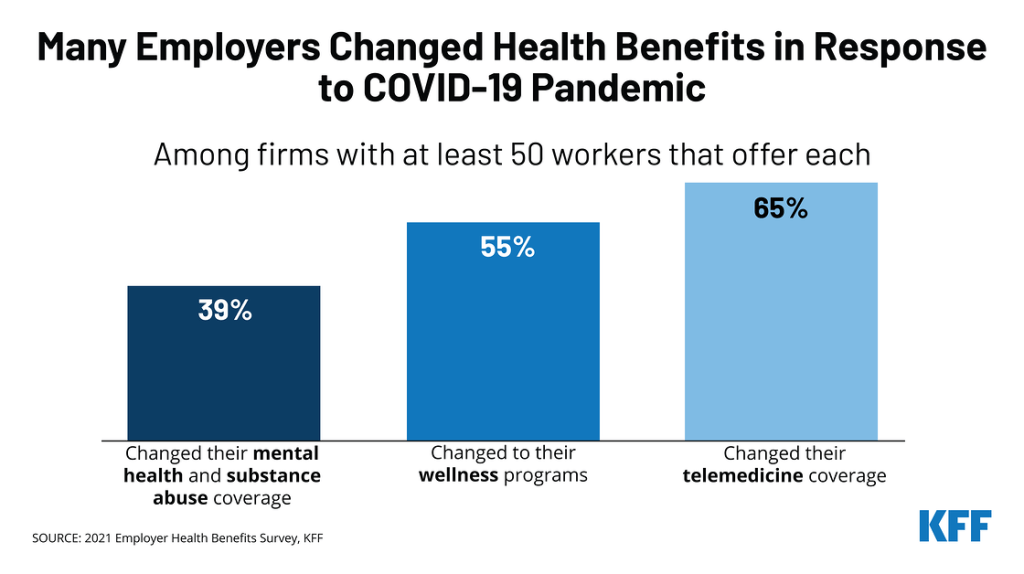
To more effectively recruit and retain talent in today’s tight labor market, many employers are updating and expanding their health benefits to better align with employees’ needs as illustrated in the recently released Kaiser Family Foundation (KFF) 2021 Employer Health Benefits Survey.
Conducted from January through July 2021, the KFF 2021 Employer Health Benefits Survey, of 1,686 randomly selected private and non-federal public employers of three or more workers, reveals how the pandemic affected workplace health benefits, including mental and behavioral health services, telemedicine, health and wellness programs, biometric screenings, and more.
Among firms with at least 50 workers that offer health benefits:
Biometric Screenings
Among firms offering health benefits, 26% of small firms and 38% of large firms provide workers the opportunity to complete a biometric screening. Among firms offering a biometric screening opportunity both this year and last year, 32% of smaller firms (50-199 employees) and 43% of larger firms report making some change in their biometric screening programs since the start of the COVID-19 pandemic. The changes include:
Read the KFF 2021 Employer Health Benefits Survey to ensure you and your clients are up to date with the latest employer-sponsored coverage data. Contact us today to develop tailored benefits solutions that address your clients’ needs.
KFF 2021 Employer Health Benefits Survey
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
New business formation soared during the COVID-19 pandemic. According to US Census Bureau data, new business applications in California increased by 20% over 2019 in 2020 to 437,000. The trend is continuing this year. That’s a lot of small group prospects that need health benefits in order to recruit employees.

The US Census Bureau has a helpful interactive chart where you can drill down to get new business formation data in your local county.
The boom in new business creation is in the news. For more information, this recent US Chamber of Commerce article provides more in-depth coverage.
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
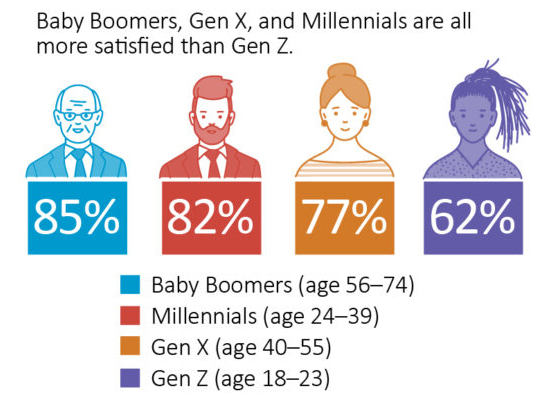
According to the results of a June 2020 American Staffing Association (ASA) Workforce Monitor® online survey conducted by The Harris Poll, more than three-quarters of U.S. employees (79%) are satisfied with their employers’ pandemic-related return-to-work plans.
Eight in 10 men (83%) compared to seven in 10 women (74%) are satisfied with such plans, while generations also differ in their satisfaction levels—with Baby Boomers (85%), Millennials (82%), and Gen X (77%) all more satisfied, and Gen Z (62%) less content.
The top five measures employees cite as critical to feeling safe at work:
However, 7% of employees said nothing would make them feel safe on the job during the pandemic, with health care workers more likely to cite this fear (14%) than those in the professional–managerial (6%) and engineering, scientific, and IT (2%) industries. One in 10 industrial (8%) and office–clerical and administrative (7%) workers also share this concern. Learn more about the ASA Workforce Monitor survey.
Confidently Advise Your Clients with Our Extensive COVID-19 Broker Resources
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Addressing employers’ cost-containment concerns and offering high-quality benefit plans tailored to their needs is simple with our quarterly Top 20 Reports.
Deliver value by offering the most economical plans to your price-conscious clients, and use our powerful Top 20 Report as a prospecting tool – if your prospect cannot afford 50% of the lowest cost plan for enrolling employees, then it’s clear they can’t afford to offer coverage.
Get Our Q4-2020 Broad and Narrow Network Plan Reports Now!
To download these must-have reports, simply submit the form on this page.
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get Industry news and exclusive updates in
your inbox, weekly.
Addressing employers’ cost-containment concerns and offering high-quality benefit plans tailored to their needs is simple with our quarterly Top 20 Reports.
Deliver value by offering the most economical plans to your price-conscious clients, and use our powerful Top 20 Report as a prospecting tool – if your prospect cannot afford 50% of the lowest cost plan for enrolling employees, then it’s clear they can’t afford to offer coverage.
Get Our Q3-2020 Broad and Narrow Network Plan Reports Now!
To download these must-have reports, simply submit the form on this page.
Questions?
Contact the small group experts at 800.696.4543 or info@claremontcompanies.com.