
To access the carrier product and rate information provided by PRISM, check the box below indicating you have read and agree to the license agreement. A button will then appear to access PRISM.
This site uses cookies to track your agreement option. If the terms of the license agreement change or if you clear the cookies from your browser, this page will appear once again during the PRISM login process.
Starting July 1, Covered California for Small Business (CCSB) is offering new Blue Shield plans, providing more options for enrollees. These plans include the Access+ HMO Network with Platinum, Gold, and Silver metal tier options, as well as the Bronze Trio HMO 7000/70. The two most popular Blue Shield High Deductible Health Plans (HDHP), Silver Full PPO Savings 2300/25% and Bronze Full PPO Savings 7000 plans, are also now available.
All of these plans offer benefits such as Wellvolution, Teladoc Mental Health, Nurse Help 24/7, LifeReferrals 24/7, and the Blue Card program for when members are outside of California.
For assistance, please contact our Quotes team at quotes@claremontcompanies.com or 800.696.4543.
Login To PrismArticle last updated: March 19, 2024.
Most of your clients likely have upcoming deadlines under the federal prescription drug benefits reporting (RxDC) requirements. Here’s a summary of the requirements, how carriers are helping, and the deadlines.
Under Section 204 of the 2021 Consolidated Appropriations Act (CAA), insurance companies and employer-based health plans must submit information regarding prescription drug benefits and health care spending. The information must be submitted to the Centers for Medicare and Medicaid Services (CMS) by June 1st of each year for the prior year’s coverage.
According to the CMS, the information that is required to be submitted by insurance companies and employers are:
Blue Shield will collect D1 Premium information from groups between February 5, 2024 and April 19, 2024. Blue Shield will also submit D2 for all groups and D3-D8 for groups with prescription drug benefits under a Blue Shield health benefit plan, and P2 accordingly. If a group does not have prescription drug benefits with Blue Shield, they should coordinate submission of D3-D8 with their pharmacy/prescription drug benefits carrier, and P2 accordingly.
Key Details
Other Details:
Information Requested
Due to technical issues on their end and updated guidance from CMS about the 2024 submission, below are revised dates:
UnitedHealthcare will complete the CAA Prescription Drug (RxDC) reporting for its fully insured and self-funded/level funded groups, including those with OptumRx as the integrated PBM. However, groups with these will need to complete the Request for Information (RFI) tool for RxDC reporting between February 1, 2024, and March 31, 2024. The March 31, 2024, deadline is firm.
To support its customers with this important filing, UnitedHealthcare will be submitting the P2 (Group Health Plan), D1 (Premium and Life Years) and D2 (Spending by Category) files for all employers who had active coverage during the reference year (2023). However, completion of the submission requires gathering some information not currently maintained in their system.
UnitedHealthcare will also submit the D3-D8 data files for customers with OptumRx as an integrated PBM. UnitedHealthcare has access to all data required to complete the submission of the D3-D8 data files. Customers who use any other PBM, including OptumRx Direct, must work with that PBM to submit the D3-D8 files.
Resources
Kaiser Permanente is required to submit information on prescription drugs and healthcare spending to CMS. On February 1, 2024 Kaiser Permanente began to send out a survey form from Kaiser-Permanente-RxDC@kp.org to all contract signers to request this information. The form must be completed by March 15, 2024.
Information Requested
Kaiser Permanente plans to submit all applicable reports and required responses for all employer groups to CMS by the June 1, 2024 deadline.
Employer groups must submit information to Sutter Health Plus regarding the average monthly premiums paid on behalf of enrollees and the amount paid by enrollees each year.
For calendar year 2023 reporting, employers or brokers are to submit the required information through the online Premium Reporting Form.
Submissions are due no later than March 1, 2024.
Cigna is reporting on behalf of Cigna + Oscar groups, so no action is required by employer groups or brokers.
Covered California for Small Business (CCSB) serves as an administrator of their participating Health Plan Issuers and is not an insurance company nor an employer-based health plan. Therefore, CCSB is not subject to RxDC data collection requirements on behalf of their employer groups. Claremont recommends that the employer follow the reporting guidelines for the enrolled carrier(s).
CCSB Resources – CCSB’s Small Business Service Center is available to help with questions at 855.777.6782.
CaliforniaChoice serves as an administrator of their participating Health Plan Issuers and is not an insurance company nor an employer-based health plan. Therefore, CaliforniaChoice is not subject to RxDC data collection requirements on behalf of their employer groups. Claremont recommends that the employer follow the reporting guidelines for the enrolled carrier(s).
The carriers are taking action to support your clients with the federal reporting requirements. In order to do so, they require information from each employer group. Look out for emails directly from the carriers, and follow their instructions. If you or your clients have questions, we can help direct you to the right contacts at the carriers.
Questions?
Contact The Answer Team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
The recent specialty plans update and reminders are listed below.
5% Dental Rate Cap Extended Through July 2021 Effective Dates
The UnitedHealthcare Dental Rate Cap Program guarantees that groups enrolling in a new plan will receive no more than a 5% increase at their first renewal.
Enhanced Dental Plan Options
Off-Cycle Specialty Adds
UnitedHealthcare allows certain specialty products to be added off-cycle without any approvals. The rate guarantee period will be adjusted so the off-cycle products renew at the policy anniversary.
Products that DO NOT require approval to be added off-cycle:
Products that DO require approval to be added off-cycle:
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
The recent specialty plan update and reminders are listed below.
Employer Bundling Program extended to July 2021 to earn up to a $3,000 credit by bundling 3+ lines of new ancillary coverage.
Qualifications
Eligibility Requirements
Download the Employer Bundling Program flyer to learn about the savings on specialty plans.
Dental and Vision Rate Passes Extended Through April 2021
Q2-2021 Small Group Rate Actions and Broker Bonus Programs
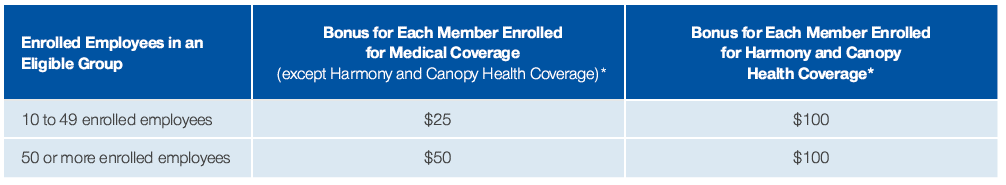
Broker bonus for new sales and renewing groups.
Specialty Benefits Quick-Quote-Tool
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
Stay up to date on the latest COVID-19 vaccination efforts by attending UnitedHealthcare’s webinar on January 27th at 12:00 pm PST.
Topics Include:
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
Prepare for Q2-2021 with these rates actions, broker bonus programs, updates, and reminders from UnitedHealthcare.
‘New’ Sales Bonus
Renewal Bonus
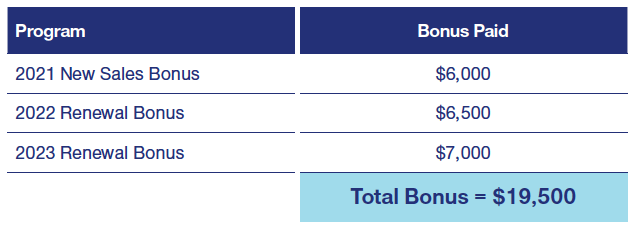
Current Small Business Broker Bonus
The current bonus program is in place and will be in addition to the bonus programs mentioned above for new groups written in 2021.
*Only agents permanently located in California are eligible for the bonus.
Choice Simplified Packages
Staff Model Guidelines
Only 5 California employees enrolled in UnitedHealthcare to offer alongside up to 2 Staff Model carriers, 60% overall participation required.
Out-of-State Guidelines
Does not require 51% to reside in a state.
Participation Certificate
Groups with 10+ employees can submit a participation certificate in lieu of a DE9C.
Start-Up Groups
6 weeks in business and 2 weeks payroll prior to the effective date.
Packaged Savings
Discounts for bundling specialty coverage (dental, vision, life and/or short-term disability) with medical coverage.
Dental
UnitedHealthcare is extending the 5% dental rate cap until July 2021 effective dates.
Vision
Motion HSA Prepaid Debit Card
HSA members (employee or spouse) can choose to receive incentives via an HSA deposit or via a prepaid debit card during Motion registration. The debit card may be used for non-health care-related expenses.
Motion and Apple Fitness+
Motion members with an Apple Watch® can now receive 5 months access to Apple Fitness+ at no additional cost from January 1, 2021 through June 30, 2021.
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
Vision Coverage
Specialty Benefits Quick-Quote-Tool
Dental and Vision Rate Passes Through April 2021
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.

Starting in 2021, UnitedHealthcare Motion® members with an Apple Watch® will be eligible to sign up for Apple Fitness+ and get a five consecutive month subscription at no additional cost.
Members will have access to Apple Fitness+ digital studio-style workouts with real-time metrics from Apple Watch synced to their iPhone, iPad or Apple TV, so they can follow their workout progress on screen. And they can choose from 10 workout types, with new workouts added every week that can be completed anytime, anywhere. Members can handpick music from their favorite artists to stay motivated. What’s more, Motion members may earn financial rewards for participating in Apple Fitness+ workouts.
Eligibility
The Apple Fitness+ promotion is available to any Motion-eligible member who activates the offer between January 1 – June 30, 2021, and has registered for UnitedHealthcare Motion and paired an Apple Watch on the UHCMotion mobile app. Once members pair an Apple Watch, they’ll receive a notification on how to redeem the Fitness+ promotion code.
Check out the press release to learn more.
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
UnitedHealthcare Specialty plan reminders:
UnitedHealthcare’s Flexible Vision Network
Enhanced Maternity and Pediatric Vision Benefits
Online Vision Providers: Warby Parker and GlassesUSA.com
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
UnitedHealthcare’s newly launched Specialty Benefits Quick Quote Tool is a web-based self-service quoting tool that allows brokers to quickly and easily provide dental, vision, and basic life quotes for groups with 2-100 eligible employees. Easily access it through United eServices using your UeS login information
New Features Include:
Check out the Quick Quote Tool guide to learn more.
Get The Quick Quote Tool Guide
Get helpful action items and definitions to review as you administer your UnitedHealthcare life and disability coverage. Download the Plan Administrator Guide.
Get The Plan Administrator Guide
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.
Attend the UnitedHealthcare COVID-19 briefing for brokers on October 21, 2020 at 10 am PDT.
Date: October 21, 2020
Time: 10 am PDT
Place: Online
Cost: FREE
Learn about:
Questions?
Contact your Claremont team at 800.696.4543 or info@claremontcompanies.com.
Get The Latest News with Text Messaging!
Your success is important to us, and we’re actively working on new solutions to support you throughout the year. To get the latest news via text messaging in the future, simply provide your cell phone number here.